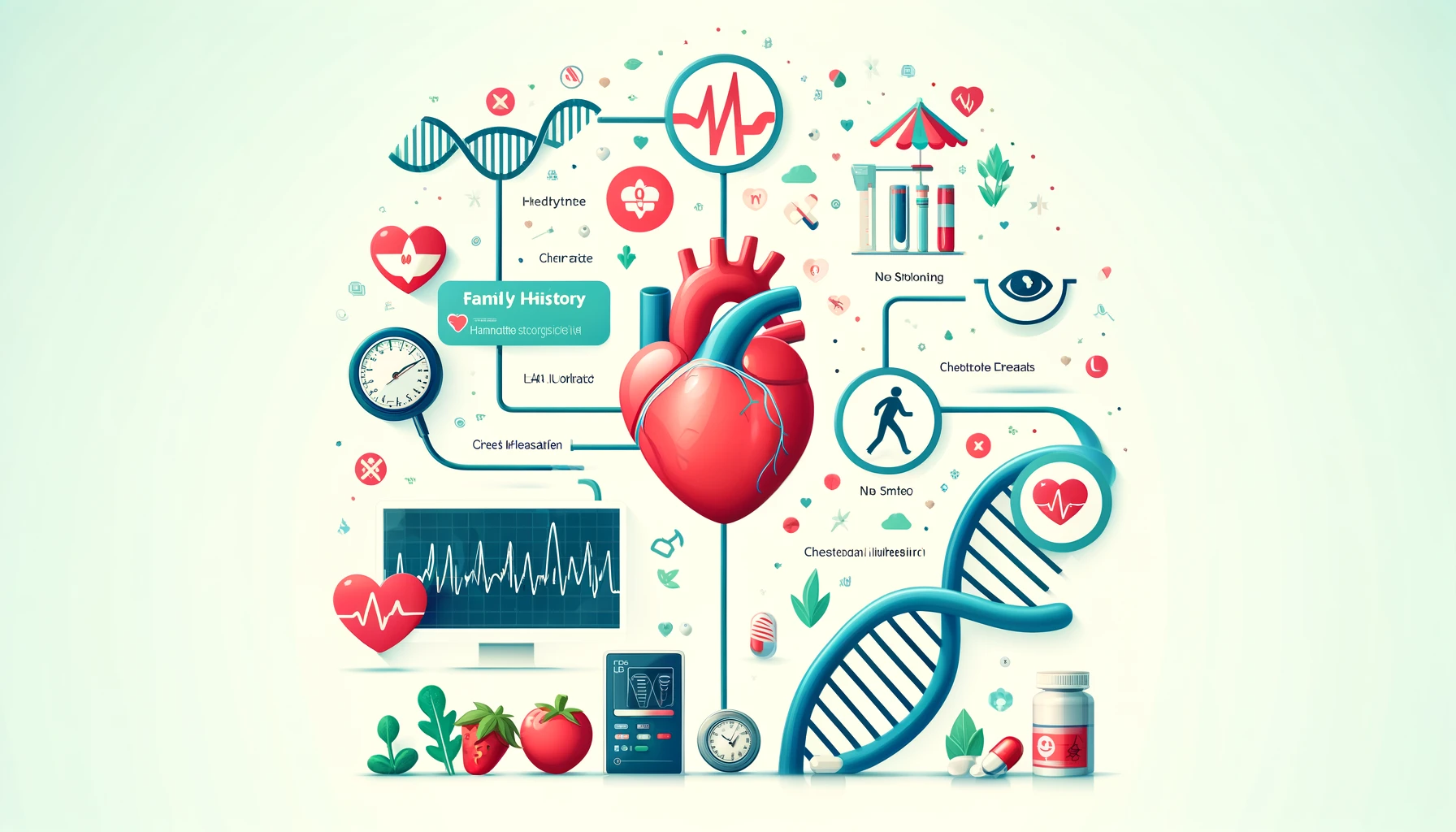
Family history of heart attack
One of the main killers on a global scale are heart attacks, sometimes called myocardial infarctions. A person’s family medical history is one of the most important elements to examine when looking at potential risk factors for cardiovascular disease. On the other hand, clinical research and lifestyle science are casting doubt on the idea that inherited tendencies cannot be changed. The essay delves at the question of whether a history of heart attacks in the family may be seen as a modifiable risk factor and offers advice on how individuals might lessen their inherited vulnerabilities.
Understanding Genetic Predisposition
Inherited genetic factors can increase the risk of heart attack if there is a history of the disease in the family. Some people are more likely to develop heart disease than others due to a hereditary tendency. Some important genetic variables have been found; however, the interaction between these genes and heart health can be complex.
Key Genetic Factors
- Cholesterol Metabolism Genes: Different people’s bodies handle cholesterol differently due to variations in genes such as LDLR, APOB, and PCSK9. Atherosclerosis, the buildup of LDL cholesterol in the arteries, is a leading cause of heart attacks, and these changes can increase levels of this “bad” cholesterol.
- Blood Pressure Regulation Genes: Blood pressure regulation is aided by genes including AGTR1, ACE, and AGT. Hypertension, often known as high blood pressure, puts extra stress on the heart and raises the probability of heart attacks, and some genetic variants can cause this condition.
- Inflammatory Response Genes: A major contributor to the onset of cardiovascular disease is inflammation. Plaque buildup in the arteries and an increased risk of heart attacks can be influenced by variations in genes such as C-reactive protein (CRP), interleukin (IL) 6, and tumour necrosis factor (TNF).
Family History and Heart Attack Risk
Having parents or siblings who have had heart attack, particularly while they were young, is a significant indicator of a hereditary risk. This trend runs in families and shows that the risk of heart attacks is greatly affected by shared environmental and lifestyle variables as well as by genetics.
Hereditary Conditions
The influence of genetic susceptibility on cardiovascular health is further demonstrated by a number of inherited disorders:
- Familial hypercholesterolemia is a hereditary condition that causes early-onset heart disease and is marked by consistently high levels of bad cholesterol (LDL) beginning in childhood.
- Hypertrophic cardiomyopathy is the abnormal thickening of the heart muscle, which makes the heart work harder to pump blood and increases the risk of heart attacks.
Epigenetics: The Link between Genetics and Lifestyle
The field of research known as epigenetics examines the ways in which environmental and behavioural variables can modify gene expression without modifying the DNA sequence. Research in this area has shed light on the ways in which lifestyle variables, including food, exercise, and stress, affect the expression of genes linked to heart attack.
Even when someone has a family history of high cholesterol, they may be able to reduce their risk by altering the expression of genes that are associated with the disease through lifestyle changes, including eating well and exercising regularly.
Epigenetic Mechanisms
- DNA Methylation: Genes can be silenced by attaching a methyl group to DNA. Methylation patterns can be impacted by lifestyle variables such as food and smoking.
- Histone Modification: Modifications to proteins that encase DNA have the ability to influence gene expression. There is evidence that exercise improves heart attack health via influencing histone changes.
- Non-Coding RNA: Personal habits impact molecules that aren’t protein-coding but can control gene expression.
Beyond Genetics: The Role of Lifestyle
Although heredity is a major component in the likelihood of heart attacks, a person’s way of life is just as important, if not more so, in deciding their cardiovascular health. Even for people with a strong genetic predisposition, an individual’s chance of getting heart disease can be significantly impacted by modifiable lifestyle choices. Taking a deeper look at the ways in which one’s lifestyle might reduce hereditary risks:
Diet: The Foundation of Heart Health
For optimal heart health, it is vital to eat a diet that is both balanced and rich in nutrients. Reducing the risk of heart disease has been consistently associated with certain eating patterns:
- Mediterranean Diet: A decreased risk of cardiovascular disease has been linked to the Mediterranean diet, which emphasises fresh produce, whole grains, lean meats (especially fish), and healthy fats (such as olive oil). There are a lot of anti-inflammatory and cholesterol-lowering nutrients in it, including fibre, omega-3 fatty acids, and antioxidants.
- Dietary Approaches to Stop Hypertension (DASH) Diet: Limiting salt consumption while boosting calcium, magnesium, and potassium consumption is the main goal of this diet. It’s a great way to reduce hypertension, which is a leading cause of heart attacks.
- Low-Carb and High-Fibre Diets: Blood sugar management, lipid profiles, and the risk of heart attack can all be improved by consuming fewer refined carbs and more fibre.

Exercise: Strengthening the Heart
A fundamental component of preventing heart disease is engaging in regular physical exercise. The heart benefits from exercise in several ways:
- Cardiovascular Fitness: Physical activities including walking, running, swimming, and cycling build aerobic capacity, enhance blood circulation, and strengthen the heart muscle.
- Weight Management: One way to lessen the strain on the heart and the likelihood of acquiring heart attack risk factors like diabetes and hypertension is to maintain a healthy weight.
- Blood Pressure and Cholesterol: By raising HDL cholesterol and decreasing LDL cholesterol, exercise helps control blood pressure and lowers cholesterol levels.
Regular aerobic exercise—either 75 minutes of vigorous effort or 150 minutes of moderate intensity—and strength training—two or more days a week—are recommended by the American Heart Association.
Smoking Cessation: Eliminating a Major Risk Factor
A major contributor to the development of cardiovascular disease is smoking. Atherosclerosis, or the hardening of the arteries caused by plaque development, is one of the health problems that can be caused by the chemicals found in cigarette smoke. There are both short-term and long-term benefits to quitting smoking.
- Immediate Benefits: Both heart rate and blood pressure decrease after twenty minutes of ceasing to smoke. Blood carbon monoxide levels return to normal after 12 hours.
- Long-Term Benefits: The risk of coronary heart attack is approximately half of what it is for a smoker one year after stopping. After fifteen years, the risk is comparable to that of someone who does not smoke.
For more content: https://iqresearcher.com/
Stress Management: Reducing the Hidden Risk
Inflammation and elevated blood pressure are two ways in which chronic stress exacerbates cardiovascular disease. Among the most effective methods for managing stress are:
- Mindfulness and Meditation: Mindfulness meditation and other similar practices have been shown to benefit cardiovascular health by lowering blood pressure, stress hormones, and tension.
- Yoga and Tai Chi: Reduce stress and enhance heart health with these mind-body exercises that include physical activity, breathing exercises, and meditation.
- Healthy Sleep Habits: Stress and cardiovascular disease are both exacerbated by insufficient sleep. Promoting heart health via prioritising healthy sleep hygiene.
Regular Health Screenings: Early Detection and Intervention
Early detection of heart attack is possible with tests that monitor critical health indicators:
- Blood Pressure: A key risk factor for heart attacks, hypertension, may be managed with regular monitoring.
- Cholesterol Levels: Early detection of excessive cholesterol levels with lipid profile testing allows both pharmacological and nutritional treatments.
- Blood Sugar Levels: Managing blood sugar levels and lowering cardiovascular risk can be achieved by screening for diabetes and pre-diabetes.
Personal Responsibility and Proactive Measures
People can greatly lower their risk of heart disease by actively addressing modifiable risk factors, even if they have a hereditary predisposition. As part of this, you need to make educated decisions regarding your food, exercise, and other lifestyle aspects.

The Interplay of Genetics and Environment
When it comes to cardiovascular disease risk, the interplay between heredity and environmental factors is intricate and ever-changing. Environmental variables and lifestyle decisions have a substantial impact on how these genetic predispositions show themselves, even if genes offer the blueprint. This section delves into the ways in which genetic risk may be modified by lifestyle choices and how environmental factors interact with genes to impact cardiovascular health.
Epigenetics: Bridging Genetics and Environment
Changes in gene expression that do not involve modifications to the DNA sequence are the focus of epigenetics, the branch of genetics that studies this phenomenon. These alterations have the potential to either increase or decrease the risk of cardiovascular disease by activating or silencing genes. Important principles of epigenetics comprise:
- DNA Methylation: Methylation is a non-sequence-altering method of modifying the activity of DNA segments. The risk of heart disease can be increased or decreased depending on methylation patterns, which can be affected by dietary factors, smoking, and toxic exposure.
- Histone Modification: Proteins called histones encase DNA. Changes in gene expression can result from changes in the chemical alterations to these histones, which impact the DNA-wrapping strength. Heart health can be improved by physical exercise and a healthy diet, which have been found to influence histone changes.
- Non-Coding RNA: Even though they can’t code for proteins, these RNA molecules have the ability to control gene expression. The amounts of non-coding RNAs can be affected by lifestyle variables including stress and food, which in turn can affect the risk of heart disease.
Lifestyle Influences on Genetic Risk
A person’s risk of heart disease and gene expression can be significantly impacted by their lifestyle choices. Several important aspects of one’s way of life interact with inherited tendencies:
- Diet: Gene expression can be impacted by nutrients and eating habits. In contrast to a diet abundant in antioxidants, fibre, and healthy fats, one high in saturated fats and carbohydrates might worsen inherited susceptibilities to inflammation and high cholesterol.
- Physical Activity: The expression of genes involved in metabolism, inflammation, and cardiovascular health can be altered by exercise. Obesity, hypertension, and insulin resistance are hereditary conditions that can be mitigated via regular physical exercise.
- Smoking: When inhaled, the chemicals in tobacco smoke alter DNA methylation patterns, leading to an upregulation of genes linked to inflammation and atherosclerosis. To lessen the likelihood of developing heart disease, quitting smoking can undo some of these epigenetic alterations.
- Stress: Gene expression associated with inflammatory and cardiovascular responses can be altered by chronic stress. These hereditary manifestations can be brought into normalcy by stress-reduction practices like yoga and mindfulness.
For more content: https://iqresearcher.com/
Case Studies: Practical Examples of Genetic and Environmental Interactions
Lifestyle decisions can impact genetic risk, as shown by real-world examples:
- Twin Studies: Environmental influences can cause differing health outcomes, according to research on identical twins. These twins share the same genetic composition. Heart disease risk can vary among identical twins due to differences in food, exercise, and smoking.
- Familial Hypercholesterolemia: High cholesterol levels typically begin at an early age in those who have this hereditary disorder. Cholesterol management and heart attack prevention are both improved in those who follow heart-healthy lifestyles that include eating well and exercising regularly.
- Hypertensive Families: The effects of lifestyle choices on families with a hypertension history might differ. In general, members’ blood pressure is better controlled when they eat healthily, exercise often, and deal with stress well.
Personal Stories: Triumph over Genetics
Getting healthy may be an inspirational and difficult path, especially for people who have a history of heart disease in their family. Success stories from people who have taken charge of their genetic predispositions show how a proactive approach to lifestyle adjustments may overcome heredity. These are some examples of such tales:
Sarah’s Journey: Overcoming Familial Hypercholesterolemia
Sarah was 30 years old when she received the diagnosis of familial hypercholesterolemia (FH). Now 45 years old, she is a mother of two. Because of her family history of the disease, she was at increased risk of cardiovascular disease due to her elevated LDL cholesterol levels. Sarah understood the need to take charge of her health due to her family’s history of early heart attacks.
Steps Taken:
- Dietary Changes: Sarah began eating more like the Mediterranean, which is high in plant-based foods, healthy fats (such as nuts and olive oil), and whole grains. She drastically cut back on saturated and trans fats in her diet.
- Exercise: Jogging, cycling, and yoga were all part of her usual exercise regimen. Because of this, she was able to keep her weight in check and her cardiovascular fitness level up.
- Medication Adherence: Sarah began taking statins at her doctor’s recommendation in order to control her cholesterol levels.
Outcome:
Sarah’s danger of cardiovascular disease diminished when her LDL cholesterol levels plummeted. Proof that careful management may lead to excellent outcomes even with a hereditary susceptibility, she has stayed heart-attack-free and continues to lead a healthy, active life.
John’s Transformation: Beating the Odds with Hypertension
Engineer John, 55 years old, came from a long line of hypertensive and heart attack sufferers. His grandpa and dad both had heart attacks when they were in their 50s. Regardless, John was hell-bent on altering his fate.
Steps Taken:
- Regular Monitoring: John started keeping note of his blood pressure measurements and began monitoring them routinely. He was able to better control his disease after an early diagnosis.
- Stress Management: John began meditating and practicing mindfulness after realising that stress was raising his blood pressure. When he needed a break, he indulged in gardening and painting.
- Healthy Lifestyle: John gave up smoking and cut back on his drinking. Along with cutting back on salt, he started eating more potassium-rich foods like bananas and vegetables by following the DASH diet.
- Physical Activity: His dedication to swimming and strength training on a regular basis allowed him to keep off the pounds and get his blood pressure down to a healthy level.
Outcome:
John was able to keep his blood pressure in a healthy level because to his hypertension management. By taking preventative measures, he enhanced his well-being and decreased his chance of a heart attack. Modifying one’s way of life may have a profound effect on hereditary risk factors, as John’s tale demonstrates.
Maria’s Success: Managing Diabetes and Heart Disease Risk
Maria, a 60-year-old former educator, has type 2 diabetes, a hereditary disorder that has raised her danger of cardiovascular illness. Maria changed her lifestyle drastically in an effort to prevent a heart attack, hoping to avert the tragedy that befell her ancestors.
Steps Taken:
- Diet and Nutrition: Maria managed her diabetes with the help of a nutritionist-designed meal plan. She advocated a diet rich in whole foods, moderate in fibre, and portion control.
- Physical Activity: She began a routine of regular exercise, which included strength training and daily walks. Because of this, she was able to control her weight and become more insulin-sensitive.
- Regular Check-Ups: Maria kept track of her glucose, cholesterol, and blood pressure readings by scheduling frequent doctor’s appointments. Consistent progress towards her health objectives was made possible by early treatments.
- Education and Support: She found emotional and practical support from others in a diabetic support group and gained insight into self-management strategies.
Outcome:
Because Maria kept her diabetes under control, she had a reduced chance of developing heart disease. She demonstrated that proactive management may result in favourable health results even when faced with a hereditary tendency by actively and happily enjoying her retirement years through her dedication to a healthy lifestyle.
উপসংহার
Even if it does increase the likelihood, having a history of heart attacks in one’s family is no guarantee. Numerous anecdotes and recent medical studies have demonstrated that one’s way of life may greatly affect how one’s genetic predispositions play out. In order to improve heart health in the long run and reduce the impact of hereditary risks, people should adopt heart-healthy behaviours, including eating a balanced diet, getting enough exercise, controlling their stress levels, not smoking, and going in for frequent checkups.
The ever-changing state of health is highlighted by the complex relationship between heredity and environmental factors. Our lifestyle choices have the power to change our genes and the dangers that are encoded in our DNA, thanks to epigenetic processes. So, even if you have a family history of cardiovascular disease, you can still take charge of your health by making educated decisions and being active.
The life-altering effects of these dietary and exercise modifications are seen in the testimonies of individuals like Sarah, John, and Maria. Despite being in increased danger due to their genes, these people have taken charge of their health and escaped the same fate as their forebears. Each of us has the capacity to seize control of our own health destiny, and these stories demonstrate that.
Finally, our lifestyle choices do affect the expression of our genes, but we can’t change our genetic composition. When people learn that having a history of heart attacks in their family is something they can change, it gives them more control over their own heart health. Making deliberate, healthful decisions allows us to drastically lower our danger of cardiovascular disease and live better, longer lives overall. Realising that our fate is written in both our DNA and the choices we make on a daily basis is the key.
Visit this link to learn more:https://pubmed.ncbi.nlm.nih.gov/3731415/


Your article helped me a lot, is there any more related content? Thanks!